In this series, we’ll share how the latest developments in this medical frontier are transforming our approaches to illness and offering new strategies to heal and prevent disease.
Previously: Short-chain fatty acids—created by the microbiome—are the main metabolites it makes that link the gut to disease.
Mind-blowing studies are revealing miraculous qualities of our gut microbes, including their ability to mediate prolific killers such as cancer and heart disease.
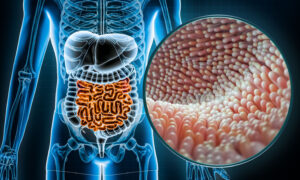
This collection of bacteria, viruses, and fungi that make up about 70 percent of our immune system has become a huge topic for researchers and authors. Hope is the latest theme in many books. It comes as research reveals gut damage from antibiotics, glyphosate, sugar, and stress can be reversed and our gut microbiome can recover. A wave of revelations over the past two decades has fed a new enthusiasm: If you nurture the bugs in your gut, they can do the work of preventing and even fighting diseases for you.
The hype that gut microbial health is human health is here to stay, according to Dr. William Li, a world-renowned physician and author. His latest book, “Eat to Beat Your Diet” focuses on metabolism, the major role of our gut microbes.
“You can see that the health of our gut bacteria has profound importance for our overall health,” Li told The Epoch Times. “These bacteria live in harmony with one another in which most of these bacteria are there for profound functions.”
One specific bacteria Li likes to highlight is Akkermansia muciniphila (A. muciniphila), which plays a role in metabolism, body weight, immune defenses, and mental well-being. It’s often found in the guts of lean people and absent in those who are obese.
Miracle Cancer Bug?
Akkermansia was identified in 2015 research as a key healthy gut bacteria that predicts a better response to cancer immunotherapy, a type of treatment that leverages patients’ own immune systems in fighting the disease.
The study, published in Science, sought to determine why only about 20 percent of patients had tremendous success with immune checkpoint inhibitors, a type of drug that signals the immune system at a cellular level. While less harsh than chemotherapy, it still has common side effects of rash, diarrhea, and fatigue. Stool samples from patients with lung and kidney cancers showed those not responding to immunotherapy had low levels of A. muciniphila. That ignited research into the microbiome’s role in cancer.
“With a good activated immune system, you’re able to take stage 3 or stage 4 cancer and reverse it to zero,” Li said. “Some of the most eye-opening research in the last five years has been in the studies of cancer patients, certain bacteria present in the gut of those responding to this powerful treatment.
“That makes gut health a matter of life and death.”
Another remarkable example that Li shared was a 2021 study in Science on advanced melanoma patients getting immunotherapy who experienced a 30 percent decrease in mortality rate for every six grams of dietary fiber they added to their diet.
“That’s profound,” he said. “What we’re finding is marvelous, incredibly mind-blowing, game-changing … but we still know so little.”
For instance, that same study found no change in the microbiota makeup of those patients increasing fiber, and it also found no benefit to adding probiotics alone. Findings don’t always match expectations.
Bugs Protecting Your Heart
Though the mechanisms are a bit complex, there is loads of evidence that metabolism in the microbiome leads to the regulation of blood pressure, cholesterol, vascular inflammation, atherosclerosis, and calcium buildup in the arteries.
“New therapeutic approaches that target gut microbes for the treatment and prevention of CVDs [cardiovascular diseases] represent exciting areas of investigation,” notes a 2020 research review in Circulation Research that links six pathways from the gut to heart disease. “Although our knowledge about how microbiota impact CVD is still rudimentary, the rate at which new discoveries are emerging is impressive.”
That same bug that plays a big role in immunotherapy, A. muciniphila, also seems to be key in reducing risks associated with heart disease, according to the research. It appears to reduce aortic atherosclerosis, a cardiovascular disease risk factor, and is being investigated as a therapeutic in human studies. In one trial against a placebo, it was found to reduce plasma lipopolysaccharide in people who were obese and had metabolic syndrome.
Lipopolysaccharides (LPS) are large molecules made of fat and polycarbohydrates that are found on half or more of the intestinal bacteria, encasing and protecting them from being digested by bile salts. But when LPS escapes the colon and crosses into the bloodstream, it becomes an endotoxin–bringing with it a storm of inflammation. LPS is a biomarker for infection in the body, and it’s used in animal studies to create an inflammatory response.
LPS is associated with heart disease and Alzheimer’s disease. There’s evidence published in the 2008 Journal of Neuroimmunology that blood plasma in Alzheimer’s patients has three times the LPS as healthy controls.
The vastness and individuality of the microbiome complicate the research. For instance, a rodent study printed in 2017 Circulation found a high-fiber diet or a microbial product could reduce blood pressure and improve heart health. However, the article referencing it pointed out most animal findings haven’t been replicated.
Of course, the microbiome is just one facet of the human immune system that plays a role in these diseases. Another part of the immune system is immune cells, and vitamin D receptors are found on almost every cell of the immune system. Before the past several years, however, there was no link found between vitamin D and the microbiome.
The Vitamin D Connection
The microbiome is largely manipulated through diet, but food is a poor source of vitamin D, which really acts more like a hormone than a vitamin in the body. There is no vitamin D receptor in the gut; however, new research is pointing to vitamin D’s role in microbiome health.
Vitamin D is naturally produced when the skin (minus sunscreen) is exposed to sunlight, especially around midday. Amid our modern indoor lifestyle, it’s more reliably increased with supplementation. It’s well-known that vitamin D decreases inflammation. Another key anti-inflammatory mechanism comes from short-chain fatty acids (SCFA), the metabolites that are made when microbes feast on fiber in the colon. SCFAs put out inflammatory fires all over the body.
Leigh A. Frame, associate director of the George Washington University Resiliency & Well-being Center, told doctors at the Malibu Microbiome Meeting that SCFAs enhance the ability of vitamin D to promote antimicrobial peptides, which are secreted by immune and epithelial cells for intestinal barrier defense. These powerful peptides bind LPS and modulate the expression of cytokines, playing an anti-inflammatory role in disease, infection, and cancer.
“One thing we do know is short-chain fatty acids enhance vitamin D to build the gut barrier,” Frame, a nutrition and microbiome expert, said.
A 2020 article in a Japanese medical journal concluded that vitamin D controls antimicrobial peptide expression, as well as modulating intestinal microbiome function, and having a protective effect on the epithelial barriers in the gut mucosa.
Another study in a 2021 special International Journal of Molecular Sciences reported that vitamin D supplementation was responsible for reducing inflammation in people with inflammatory bowel disease (IBD), as well as improving the makeup of the microbiota.
Gut Diseases and Disruptions
Gut diseases such as IBD are illnesses of Western civilization—not a function of genetics but a function of a lifestyle marked by chemical exposures and disruptions to the gut barrier, according to Dr. Ari Grinspan, associate professor of medicine and director of the fecal microbiota transplant program at Mount Sinai Hospital.
He told The Epoch Times that there’s promise on the horizon that changing the makeup of the microbiota can have a significant impact on serious diseases.
“There’s so much potential. We have to be cautiously optimistic. A lot of these things are not going to pan out,” he said. “But maybe there will be a subset of these patients that we can help by using alterations in the microbiome. That’s why I’m very excited about where this leads us in the future.”
Next: How do you know if you are at risk for microbiome-related diseases? It’s not always obvious, but a personal inventory of toxins, body mass, and sleep offer clues.
Read Part 1 – Killing Bacteria with Antimicrobials and Antibiotics May Be Shortsighted, According to New Science About the Microbiome
Read Part 2 – How the Gut Cures and Creates Disease
Read Part 3 – Why Scientists Are Obsessing Over the Bugs in Our Stool
Read Part 4 – Decoding Dysbiosis: Are Your Gut Microbes Out of Whack?
Read Part 5 – Our Gut Bugs Make Tiny Metabolites That Have Gigantic Jobs
Profile of a Top Bug
Akkermansia muciniphila bacteria make up 1 percent to 5 percent of total species in the gut microbiome. It triggers an increase of goblet cells in the gut lining, which create mucus and strengthen the intestinal barrier. Low levels of this bacteria are associated with increased intestinal permeability.
Akkermansia also produces acetate and propionate, two anti-inflammatory short-chain fatty acids. Low levels are linked to obesity, fatty liver disease, and cardiometabolic disorders. In most autoimmune diseases, Akkermansia levels are low, but there are a few exceptions, including psoriasis and Type 1 diabetes. In other diseases, including Crohn’s disease, eczema, rheumatoid arthritis, and multiple sclerosis, there are conflicting studies and information.
Those studies are outlined in Dr. Akil Palanisamy’s book, The T.I.G.E.R. Protocol: An Integrative 5-Step Program to Treat and Heal Your Autoimmunity, which highlights five keystone gut bacteria. Palanisamy also wrote about a three-month trial with oral Akkermansia that found it improved insulin sensitivity and decreased body weight, fat mass, liver inflammation, and hip circumference in overweight adults. He added that foods rich in red polyphenols, such as berries and red cabbage, can help raise levels. So can intermittent fasting.
Information adapted from The T.I.G.E.R. Protocol by Akil Palanisamy, MD. Copyright © 2023 by Akil Palanisamy, MD. With permission from Balance, an imprint of Grand Central Publishing. All rights reserved.

0 Comments :
Post a Comment